In almost every extended family in Ghana, there’s someone living with sickle cell. And if not, it’s likely because they don’t even know yet.
That’s how close this condition hits home.
Sickle Cell Disease isn’t rare in Ghana. In fact, Ghana is one of the countries with the highest number of people affected. According to the Ghana Health Service, about 15,000 babies are born with sickle cell disease every year. That’s roughly 40 babies every single day starting life with this lifelong condition.
And yet, many people still don’t have enough information on sickle cell management in Ghana: what it is, how it works, or how it can be managed properly. That’s exactly why this guide exists — to break it all down in simple language anyone can understand.
What is Sickle Cell Disease?

Sickle Cell Disease (SCD) is a genetic blood disorder. That means you’re born with it — it’s passed down from your parents through their genes. It’s not contagious, and you can’t “catch” it later in life.
In simple terms, sickle cell affects your red blood cells — the part of your blood that carries oxygen around your body.
Normally, red blood cells are soft and round, like doughnuts. But in someone with sickle cell, some of these cells become hard and shaped like a sickle or a curved banana.
These oddly shaped cells:
- Don’t move easily through small blood vessels
- Break apart more quickly
- Block blood flow, causing pain and damage to organs
What causes it?
It happens when a person inherits the sickle cell gene from both parents. If you get the gene from only one parent, you have what’s called the sickle cell trait — you won’t have the disease, but you can pass the gene on to your children.
This is why knowing your genotype before starting a family is so important — two carriers (AS + AS) have a 25% chance of having a child with sickle cell disease (SS).
Types of Sickle Cell Disorders
Yes, there’s more than one.
The most common types include:
- HbSS – This is the most severe form and what most Ghanaians refer to when they say someone has sickle cell.
- HbSC – A milder form but still with health complications.
- HbS Beta Thalassemia – Less common but also affects how red blood cells behave.
In Ghana, HbSS and HbSC are the most frequently seen types.
What are the symptoms?
Symptoms can vary from person to person. Some may experience mild issues, while others have frequent complications. Common signs include:
- Fatigue and weakness (because fewer healthy red blood cells means less oxygen)
- Frequent pain episodes (called “crises”) usually in the chest, joints, or back
- Swollen hands and feet in babies
- Delayed growth or puberty
- Frequent infections
- Yellowing of the eyes (jaundice)
In Ghana, these symptoms are sometimes mistaken for other things like malaria or “body weakness,” which leads to delays in proper treatment.
Sickle Cell Prevalence in Ghana: The Current Situation
If you’re in Ghana right now, there’s a high chance you know someone with sickle cell — or you might even be living with it yourself. That’s how common it is.
Sickle Cell Disease (SCD) is one of the most widespread genetic conditions in Ghana, and understanding just how serious it is can change the way we approach testing, support, and treatment.
National Statistics: How Common is Sickle Cell in Ghana?
Behind every statistic is a family: a child in pain, a mother overwhelmed, or a young adult unsure about marriage and children. Sickle cell management in Ghana starts with awareness. And awareness begins with knowing how big the problem truly is.
Now here’s the hard truth: About 2% of all babies born in Ghana each year have Sickle Cell Disease. That’s approximately 15,000 children every year, or over 40 babies every single day starting life with a lifelong health condition.
And it doesn’t stop there.
Roughly 25% of Ghanaians (1 in 4) carry the sickle cell trait (AS), which means they can pass it on to their children even if they don’t have symptoms themselves.
That’s a huge number — and a clear reason why genotype testing should be as normal as checking your blood pressure.

High-Risk Groups in Ghana
While anyone with the genetic combination can have sickle cell, some groups face higher risks and challenges, especially:
- Newborns and young children, due to limited early screening
- People in rural areas, where access to healthcare and testing is limited
- Couples who both carry the AS trait, but are unaware of it
- Low-income families, who may struggle to afford consistent care
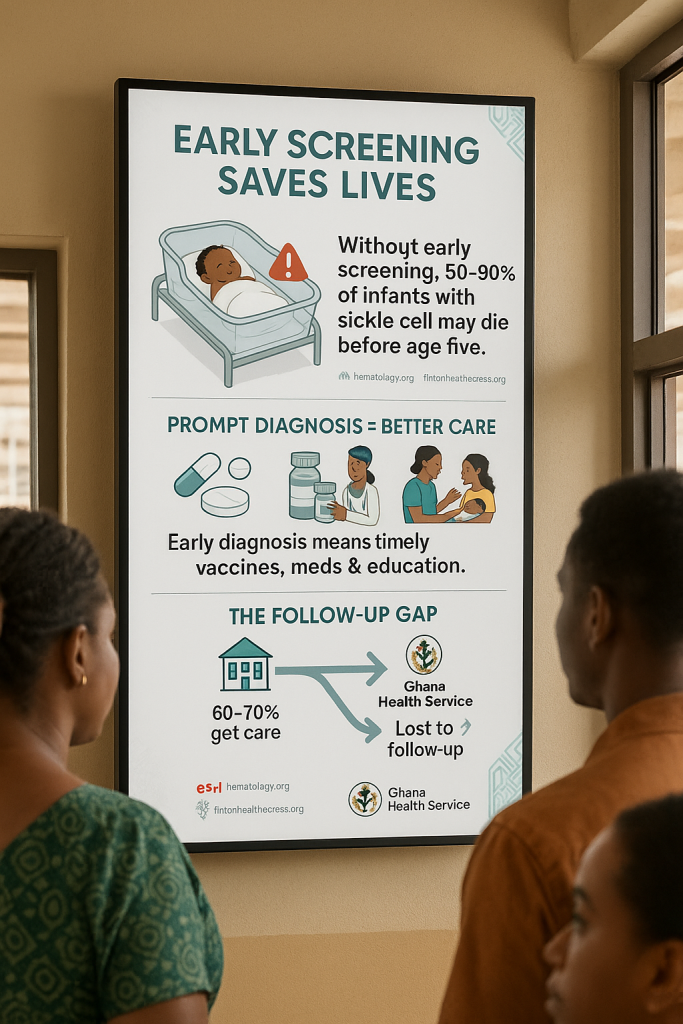
Early diagnosis is still not universal across Ghana, and many children are only diagnosed after a severe health crisis, which delays treatment.
Regional Variations: Where Is It More Common?
Sickle cell isn’t evenly spread across Ghana. Certain regions report higher rates than others, often due to population size and awareness levels.
A study by the National Library of Medicine looked at hospital records in Ghana from 2012 to 2017 to understand what affects how long sickle cell patients stay in the hospital.
Out of over 22,000 cases, the study found that younger patients and those with other health conditions tended to stay longer. It also showed that some regions—like Volta and Eastern—had more cases, while places like the Northern and Upper East regions had fewer. These findings highlight the importance of early screening and better healthcare planning, especially in areas with a higher number of sickle cell cases.
Unfortunately, exact regional breakdowns are still limited, as not all births are screened, and many cases go unreported. But one thing is clear: no region is untouched.
Diagnosing Sickle Cell in Ghana
Newborn Screening Programs
Ghana rolled out its first newborn screening pilot in 1993 in Kumasi and Greater Accra, but coverage was limited back then. Over time, the program expanded.
With support from CHAI and the Gates Foundation, 14 more screening sites were added by 2023, bringing the total to 11 of 16 regions offering newborn screening.
By mid-2023, over 24,000 infants had been screened; about 397 tested positive, and 204 were successfully linked to care. Still, only around 1 in 18 babies born get screened, meaning many are either missed or are diagnosed late during an emergency.
How Testing is Done
Testing is quick and painless. Here’s how it works:
- A heel prick collects a few drops of blood on a special card (a dried blood spot).
- Samples are shipped to labs—most often at the Noguchi Memorial Institute—where technicians run hemoglobin electrophoresis to identify the specific sickle cell type.
- Results typically come back within a few weeks. If positive, the child is referred to a specialist sickle cell clinic.
- Those diagnosed are quickly enrolled in a care program, starting penicillin, vaccinations, and counseling for families.
At big hospitals like Korle Bu, screening has grown from covering only 44% of newborns in 2017 to about 84% as of 2019.
Where to Get Tested in Ghana
- Public Hospitals: Major maternity wards in Accra, Kumasi, and Tamale routinely offer sickle cell screening. These include Korle Bu Teaching Hospital, 37 Military Hospital, and Komfo Anokye Teaching Hospital
- Regional Health Facilities: Many now have newborn screening, especially in the Greater Accra, Ashanti, and Northern regions
- Private Labs and Clinics: Establishments like SYNLAB in Accra offer testing for a fee.
- CONSA-supported Sites: Under the American Society of Hematology’s project, hospitals such as 37 Military and Greater Accra Regional Hospital now include routine screening
However, newborn screening isn’t 100% universal yet—rural clinics and home births are often left out, delaying diagnosis until symptoms flare up.
While Ghana has come far from its early pilot days, we still have a way to go to ensure every baby is tested and treated on time.
The tools are there—heel prick tests, labs, trained nurses—but rolling them out everywhere, especially rural areas, remains vital.
Treatment Options for Sickle Cell Patients in Ghana
When a pain crisis hits, these basic treatments matter most—and they’re often the first line of defense.
Pain Management
When sickle cells block blood flow, severe pain — called a “crisis” — often follows. In Ghana, care usually starts with:
- Oral painkillers and bed rest at home, if your crisis is mild.
- Hospital-based care when pain is “unmanageable”—this includes IV fluids, oxygen, and stronger painkillers like opioids.
Hospitals and clinics are gradually adopting standardized pain protocols, which aim to start effective pain relief within 30 minutes of arrival. Fast response like this significantly shortens hospital stays and eases suffering.
Hydroxyurea Therapy
This is a game-changer—and good news: it’s now more accessible in Ghana.
- The Ghana Food and Drug Authority approved hydroxyurea for all ages in 2018
- The Ministry of Health and healthcare partners rolled out hydroxyurea through public-private partnerships and included it under the National Health Insurance Scheme.
- Recently, CHAI and Qilu Pharma introduced generic versions at reduced cost, making the medication more affordable for families
Studies show hydroxyurea:
- Increases fetal hemoglobin
- Reduces pain crises, hospital visits, and need for blood transfusions.
According to the SickleInAfrica registry, about 21% of Ghanaian sickle cell patients are on hydroxyurea, the highest rate in West Africa. But despite progress, many still face cost and monitoring barriers, including regular blood tests.
Blood Transfusions
Transfusions can be lifesaving during crises, severe anemia, or to prevent stroke. In Ghana:
- They’re used in acute settings and to boost hemoglobin before surgery, when the doctor recommends.
- However, blood supply is limited—multiple units may be needed, and shortages are common.
- Hydroxyurea can help reduce the need for transfusions—a key benefit given blood scarcity.
Bone Marrow Transplant (Stem Cell Transplant)
This is currently the only potential cure, but it’s still rare in Ghana:
- Requires a matched donor (usually a sibling), expert medical teams, and labs.
- A few centers, such as Korle Bu Teaching Hospital, have explored it in partnership with international bodies
- It’s high-cost and high-risk, often out of reach for most families.
However, global advances in gene therapy and less intensive transplants promise future possibilities, although affordability and infrastructure remain hurdles.
Access & Affordability Challenges
No matter how effective a treatment is, if it’s out of reach, its impact is limited:
- Hydroxyurea still carries costs, and insurance coverage—while improving—doesn’t always cover lab tests needed for safe use.
- Blood transfusions also come with costs and supply challenges in rural areas.
- Families report ongoing financial strain from repeated clinic visits, medications, lab fees, and travel, even with insurance.
To truly improve sickle cell management in Ghana, we need broader access, stronger healthcare systems, and fair pricing—so every person with SCD can live healthier, longer lives.
Daily Management and Lifestyle Tips for Sickle Cell Patients

A simple routine is more than mindfulness—it’s part of the daily battle plan against sickle cell. Small habits like these can make a big difference:
Nutrition and Hydration
Think of your body like a well-oiled machine—it needs quality fuel and plenty of fluids to run smoothly. Here are a few tips to keep in mind:
- Hydrate regularly: Aim for 8–10 glasses of water a day, even more when you’re out in the heat or feel unwell. Staying hydrated helps prevent painful “crisis” episodes by keeping blood thin and flowing smoothly.
- Eat a balanced diet: Include leafy greens, fruits, lean proteins, and healthy carbohydrates at every meal. This variety supports strong immunity and helps replenish nutrients lost with each sickle cell crisis .
- Supplements can help: Your doctor might prescribe folic acid, B-complex vitamins, or penicillin—stick with them to keep red blood cells healthy and infections at bay.
Avoiding Triggers
SCD isn’t just a state of being—it’s a condition triggered by everyday stresses. Taking care of yourself can greatly reduce painful episodes.
- Pay attention to temperatures: Avoid sudden exposure to very hot or cold environments—Ghana’s weather can be unpredictable, especially early in the rainy season.
- Limit intense activity: Stay active, but steer clear of heavy exertion without proper hydration and rest.
- Minimize alcohol & caffeine: Drinks like alcohol and strong tea can dehydrate you. Opt for water or natural fruit juices instead.
- Manage stress: Emotional stress itself can spark a crisis. Simple relaxation—like deep breathing, listening to music, or gentle rocking—can make a huge difference.
Preventing Infections
People with SCD are more likely to fall sick and fast. Staying healthy means staying protected.
- Stay up-to-date with vaccines, including flu, pneumococcal, and COVID-19 shots.
- Take daily penicillin (usually until age five, but sometimes longer for more severe SCD).
- Practice good hygiene: Wash hands, keep wounds clean, and always use safe food-handling practices.
- Steer clear of illness: Avoid people with coughs, colds, or flu—wearing a mask or staying home when sick can protect your whole household.
- Guard against malaria: If you’re in a mosquito zone, use nets, repellents, and follow your doctor’s advice on preventive medicine.
Managing Fatigue
Feeling tired isn’t just in your head—it’s a normal part of SCD. Here’s how to handle it with care:
- Stick to a sleep routine: Go to bed and wake up at the same time each day. Limit screen time before bed and keep your room peaceful.
- Power naps: Short naps (20–30 minutes) can help restore energy. Just don’t nap too late in the day.
- Know when to rest: When your body starts telling you it’s tired, slow down, hydrate, and let yourself rest.
- Pace daily tasks: Break chores into smaller steps and spread them out to avoid tiring yourself out.
Quick Daily Checklist
- Drink water regularly—carry a refillable bottle
- Eat balanced meals full of colour and nourishment
- Dress for the weather—stay warm and cool as needed
- Take medications and supplements on schedule
- Keep vaccines up-to-date and follow penicillin plans
- Wash your hands and avoid close contact with the sick
- Stick to a sleep plan and rest when necessary
These everyday habits won’t cure SCD, but they help you live better, avoid crises, and keep your health on track.
Mental Health & Emotional Support for Sickle Cell Patients
Living with sickle cell means carrying a lot more than physical pain—it often brings emotional stress that deserves understanding and care.
Facing a Chronic Illness Day by Day
Dealing with sickle cell isn’t just about treating pain—it’s managing constant uncertainty. Frequent hospital visits, missed school or work, and health setbacks can bring feelings of worry, sadness, isolation, or even guilt.
Studies in Ghana have shown that psychological distress isn’t highly common, but those with the most severe forms (like HbSS) may experience more depression, anxiety, and painful emotional burdens.
Every emotional hardship matters, and it’s exactly why families supporting loved ones with sickle cell play a crucial role.
Finding Help Through Counseling Services
Professional counseling can be a game-changer. For adolescents, especially, talking through worries, learning coping strategies, and building resilience can really improve quality of life.
A counselor or therapist can offer tools for techniques like cognitive-behavioral therapy (CBT), helping patients break negative thought patterns, manage pain-related stress, and strengthen mental well-being.
Schools, hospitals, or private clinics in larger cities now offer tailored services, though awareness and access still need improvement.
Connecting with Others: Support Groups in Ghana and Online
- In Ghana, hospital-run groups and nonprofit sessions let patients and families share stories, ask questions, and break the silence around sickle cell health.
- Online, global communities—like the Sickle Cell Disease Association’s mental health toolkit—offer remote peer support and expert advice, especially helpful during flare-ups or emotional lows.
Even just knowing you’re not the only one feeling this way makes a big difference.
Why Emotional Support Matters
| Benefit | How It Helps |
|---|---|
| Better disease management | Reduces stress, improves pain control, and overall health |
| Fewer crises | Emotional stability can help lessen trigger-driven flare‑ups |
| Stronger life outlook | Boosts resilience and motivation to stay on treatment plans |
Healthcare pros emphasize that care for sickle cell patients must include psychological and social support, not just medical treatments.
Building emotional support isn’t just nice—it’s essential. When patients feel heard, understood, and equipped to cope, they live better—physically and emotionally.
Government and NGO Support Programs in Ghana
Tackling sickle cell in Ghana is not just about medicine; it’s also about systems, support networks, and strong advocacy. Here’s how both the government and NGOs play vital roles.
National Sickle Cell Programs
- Newborn screening program: Launched in the early 1990s, this initiative has significantly expanded with support from the Ministry of Health, Ghana Health Service, and partners like CHAI. As of 2023, over 24,000 infants have been screened across 14 sites in 10 regions, leading to early diagnosis and linkage to care.
- Inclusion of hydroxyurea in NHIS: Since 2022, hydroxyurea—an essential disease-modifying therapy—has been covered under Ghana’s National Health Insurance Scheme (NHIS), thanks to collaboration between the government, Novartis, and the Sickle Cell Foundation of Ghana.
- National Strategy & Policy Alignment: The government, backed by international guidelines like WHO’s Sickle Cell Disease Package, has introduced national strategies and data systems across regional hospitals to improve screening, diagnosis, and treatment.
NGOs and Foundations Providing Assistance
- The Lord’s Blessings Foundation: Based in Kumasi, this grassroots organization supports individuals and families through education, emotional support, and community advocacy for sickle cell care.
- Sickle Cell Foundation of Ghana (SCFG): Since 2004, SCFG has led national awareness campaigns, offered support services, and advocated for better patient care. With Novartis’s support, they’ve helped equip over 100 clinics and trained health staff to enhance sickle cell disease care across Ghana.
- Sickle Cell Condition Awareness Advocates (SICCA): This group pioneered Ghana’s first pre-conception screening project in collaboration with the Ghana Academy of Arts and Sciences, helping couples make informed family planning decisions.
Sickle Cell Prevention in Ghana: What Can Be Done?

Genetic Counseling
Genetic counseling helps you understand your chances of passing on sickle cell before starting a family. Counselors take your family history, explain inheritance patterns, discuss lab testing, and support your decision-making.
In Ghana, a key study found young adults are open to genetic counseling, but many don’t know where to go. That gap shows the need for more counselors and better awareness. Programs like those at the University of Ghana and training opportunities aim to close it.
Public Awareness Campaigns
Knowledge is powerful. The World Health Organization promotes public education and genetic counseling as essential for preventing sickle cell. In Ghana, church leaders, schools, and NGOs are joining forces.
Ideas include presenting genotype talks at youth groups, organizing community screenings in churches and mosques, and launching media campaigns to increase awareness.
Studies show a strong link between awareness and proactive behavior — when people know their status, they’re 0.7 times more likely to get screened before marriage. Effective campaigns mean better-informed decisions.
Premarital Testing
Screening before marriage is one of the most cost-effective ways to prevent SCD. In many African countries, around 48% of couples choose to do this before tying the knot.
Ghanaian college students are generally supportive, though only about 12% actually go for screening.
In Ghana’s Ahafo Region, 89% of young adults said they’d like premarital screening, but only 14% had acted on it. Clearly, awareness isn’t enough—programs must offer accessible, affordable testing and strong encouragement.
Why These Steps Matter
| Preventive Step | Why It Matters |
|---|---|
| Genetic counseling | Offers personalized risk info, empowers couples |
| Awareness campaigns | Normalize talking about sickle cell and testing |
| Premarital screening | Helps couples plan and reduce risk of SCD children |
Working together—health ministries, clinics, religious leaders, schools—can make these prevention steps common practice in Ghana. It’s not just a medical win; it’s about giving families peace of mind.
Conclusion: The Path Forward for Sickle Cell Management in Ghana
Sickle cell disease remains a significant public health challenge in Ghana, but with the right information, early diagnosis, family support, and consistent care, many patients can live healthier and longer lives.
This guide has explored what sickle cell is, how it’s diagnosed, treated, and managed daily, and the crucial roles government, NGOs, and families play. Yet beyond medicine, we must confront the stigma that isolates patients and prevents open conversations. Sickle cell is not a curse—it’s a condition that deserves compassion, not judgment.
Ghana’s progress depends on continued education, stronger policies, and community-led advocacy. Let’s make that future possible. Support the work of The Lord’s Blessings Foundation today—your help can spread life-saving education, reduce stigma, and bring hope to sickle cell warriors across Ghana.
FAQs
Can sickle cell skip generations?
No. Sickle cell doesn’t skip generations—it only appears when both parents carry the sickle cell gene (usually AS). If only one parent is a carrier, the child won’t have the disease.
What is the life expectancy for someone with sickle cell?
With proper care, people with sickle cell in Ghana can live into their 50s or beyond. Early diagnosis, treatment, and a healthy lifestyle can significantly improve life expectancy.
Can you have children if you have sickle cell?
Yes. Many people with sickle cell have children. However, pregnancy can be high-risk, so medical support and genetic counseling are important for planning and safety.
Is it safe to travel with sickle cell?
Yes, but with precautions. Stay hydrated, avoid extreme temperatures, and prepare for altitude changes. Always carry medication and have a medical plan in place.
What triggers a sickle cell crisis?
Common triggers include dehydration, infections, extreme temperatures, stress, fatigue, high altitude, and smoking. Sometimes, crises happen without warning—so daily care and awareness help reduce risk.